The Hernia is an outward bulge in the abdomen. In which part of the liver, intestine or fatty tissue is protruded through the abdominal wall defect.
The success rate of surgery for Laparoscopic Hernia Dubai is very high. There are a variety of different types of hernias, depending on their abdominal position, including:
- Ventral Hernia
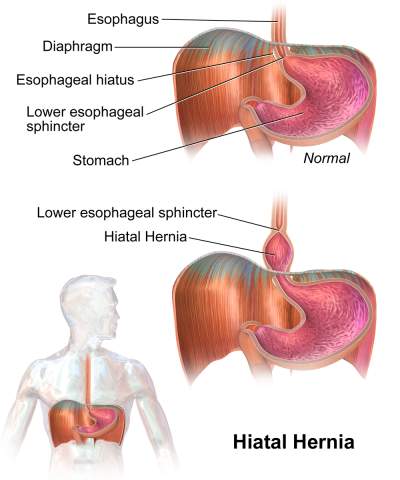
- Hiatal Hernia
- Femoral Hernia
- Inguinal Hernia
- Umbilical Hernia
Laparoscopic hernia signs and symptoms
The bulge formed after hernia protrusion may become painful and repeats after coughing, erecting or lifting heavy items.
Some signs and symptoms of Laparoscopic Hernia Dubai are:
- Constipation
- Diarrhea
- Faster Heartbeat
- Fever
- Continuous pain near the hernia region
- Nausea or vomiting
Laparoscopic Hernia Causes:
The main cause of all cases of hernia is the weakening of the abdominal wall, either as a birth defect or later in life.
The lining of the abdomen has natural areas with a potential weakness. Hernias may develop in these or other areas as a result of severe pressure on the abdominal wall, age, injury, old incision, or birth weakness.
Anybody can develop a hernia at any age. Most of the hernias of infants were congenital. For adults, a normal weakness or pressure from heavy lifting, excessive coughing, difficulties for bowel movements, or urination can cause the abdominal wall to fade or split.
What is the required preparation in Laparoscopic Hernia Dubai?
Most laparoscopic hernia in Dubai treatment is done on an outpatient basis, so you are able to go home on the same day that the operation is performed. Preoperative training requires blood work, medical assessment, and EKG based on your age and medical condition.
Once the specialist reviews the possible risks and benefits of surgery for you, you will need to provide written consent for surgery.
At midnight the night before surgery, you should not eat or drink anything except drugs that your surgeon has told you are allowed to take with a sip of water in the morning of surgery.
Medications such as aspirin, blood thinners, anti-inflammatory medications (arthritis drugs) and vitamin E may need to be immediately halted for several days to a week prior to surgery.
The specialist will discuss this with you and offer guidance about your drugs around the time of surgery. It is advised that you shower the night before or in the morning of an antibiotic soap operation.
How is the procedure performed?

There are few options available for a patient with a hernia.
The use of a truss (hernia belt) is seldom used because it is generally unsuccessful. It may ease any pain but does not eliminate the risk of incarceration or strangulation of the intestines.
Most of the hernias require surgery. Surgical procedures are conducted in one of two ways:
- An open route is done from the outside through a three or four-inch incision in the groin or hernia region. The incision should extend through the tissue, subcutaneous fat, and allow the surgeon to reach the level of the defect. The surgeon may choose to use a small part of the surgical mesh to patch the defect or the hole. This technique can be performed with local anesthetic and sedation using a spinal anesthetic or general anesthetic.
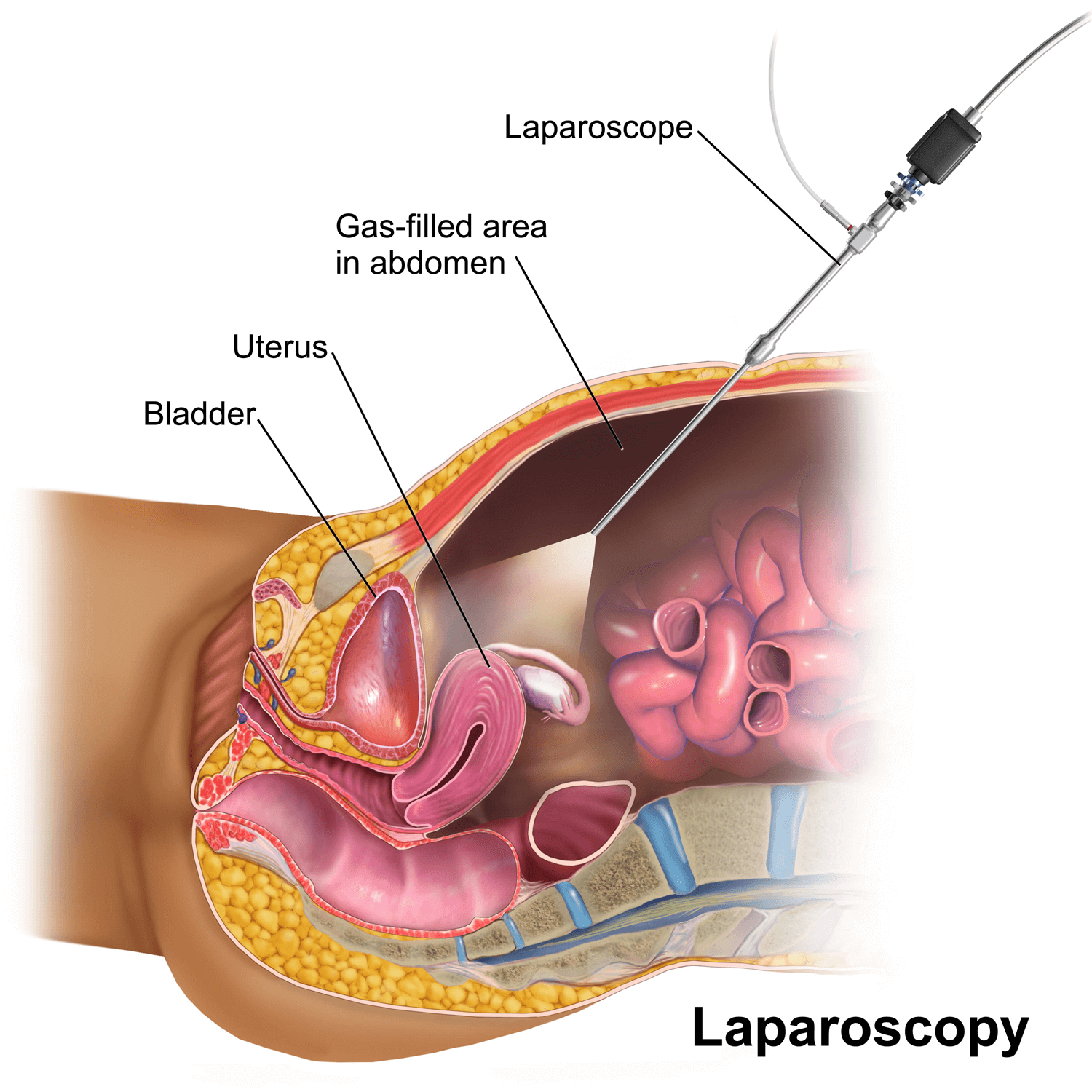
- The laparoscopic hernia treatment is done using a laparoscope (a tiny telescope) attached to a special camera, which is implanted into a cannula, a thin hollow tube, enabling the surgeon to view the hernia and underlying tissue on a video screen.
Dr. Muharrem Oner performs the best Laparoscopic Hernia surgery in Dubai. He had an unmatched experience of hernia treatment for more than 15 years.
The complications that can come during Laparoscopic hernia surgery Dubai
- Any surgery may be fraught with complications. The main complications of any surgery include vomiting and inflammation, which are rare for the treatment of laparoscopic hernia.
- There is a very small risk of injury to the urinary bladder, intestines, blood vessels, nerves, or sperm stream that leads to the testicle.
- Urinating complications after surgery may arise and may include the insertion of a catheter or tube to empty the bladder after surgery. You can ask the physician how you can prevent this from happening before your surgery.
- Bruising and inflammation of the scrotum, the base of the penis, and the testicles are not rare for open and laparoscopic replacements.
- It can come back any time a hernia is patched. This long-term recurrence rate is low in patients undergoing laparoscopic repair by experienced surgeons. The surgeon will help you decide if the chance of treating laparoscopic hernia is less than the risk of leaving the disease untreated.
- It is very important to remember that before going for any type of surgery–whether laparoscopic or open, you should ask your surgeon about the experience he had with the operation.
Do I need a Laparoscopic Hernia Dubai Treatment?
The doctor will probably prescribe you that if any of these things happen to you or not:
The tissue (such as the intestine) is stuck in the abdominal wall. It's called prison. When left untreated, this may lead to strangulation. This is when the blood supply to the skin is closed short.
The hernia is strangulated. This can lead to permanent injury and is a medical emergency. Strangulated tissues, normally the intestines, may fail, and if you do not extract them soon, you may become seriously ill.
Call your doctor right away if you have a fever or diarrhea, a sharp pain that is getting worse, or a hernia that turns red, purple, or black.
Hernia causes pain or discomfort, which grows larger.


_medium.jpg)




 One adrenal gland sits above each of your kidneys. Your two adrenal glands produce various hormones that help regulate your metabolism, immune system, blood pressure, blood sugar and other essential functions.
One adrenal gland sits above each of your kidneys. Your two adrenal glands produce various hormones that help regulate your metabolism, immune system, blood pressure, blood sugar and other essential functions.